Obsessive-compulsive disorder (OCD) is an incredibly debilitating mental health condition that affects individuals in various ways, including compulsive behaviours like reassurance-seeking and accommodation behaviours.
When someone with OCD is suffering, it’s natural for loved ones to want to help. However, while adhering to these reassurance-seeking and accommodation behaviours may reduce distress in the short term, some of the things our loved ones ask us to do may over time actually reinforce OCD patterns. The good news is that there are ways to offer long-term support and not reassurance.
This article will explain how reassurance-seeking and accommodation behaviours manifest, why they can be harmful, and most importantly, how you can help your loved one break free from these OCD-driven patterns.
What are reassurance-seeking and accommodation behaviours?
Similar to how intrusive thoughts are something everyone experiences, seeking reassurance is a very normal reaction to situations of worry or doubt. But for someone with OCD, this need to seek reassurance may be the only way they are able to relieve the anxiety caused by their intrusive thoughts.
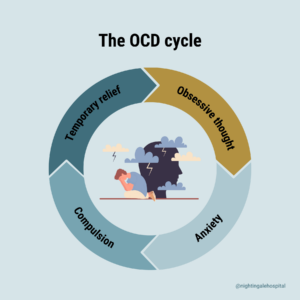
The OCD, anxiety and reassurance-seeking cycle is helpful to understand the how your loved one might be feeling, and also the ways in which you might be able to help break this cycle, or help your loved one to recognise this cycle in their own thoughts.
First, your loved one’s anxiety is triggered. There are many things that might trigger this anxiety but for this example let’s say your loved one is worried if they locked the door on their way out. In direct response to this trigger, your loved one will likely ask for reassurance. A normal reaction to this scenario would be to provide that reassurance, saying something like, “I checked that it was locked.” This will provide the temporary relief that your loved one is looking for. But this initial relief from the anxiety does not keep the anxiety completely at bay. Eventually, the doubt will resurface, or it might be replaced with another one will take its place. And so the cycle continues.
Accommodations for OCD are when you might participate in your loved ones rituals or help them avoid situations or places that provoke anxiety.
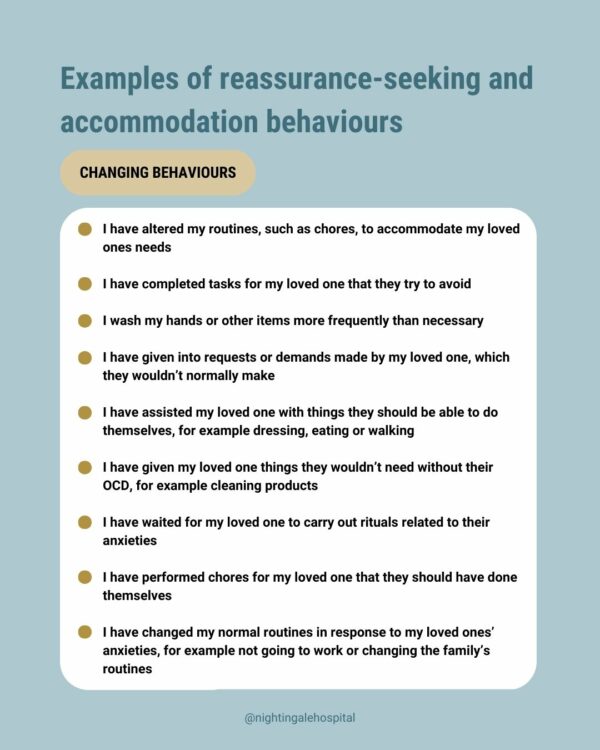
Examples of reassurance-seeking and accommodation behaviours
We want to be very clear that providing reassurance to or engaging in accommodations with your loved one is a very normal reaction to the anxiety they’re feeling. We don’t give these examples to deepen any guilt or shame you might feel about the ways you have given reassurance to your loved one, or even the situations that you tried to not give reassurance. Instead, we provide these examples because they’re likely situations you are all too familiar with and it can be helpful to understand that these reactions are completely human.
Avoidance
- I have helped my loved one avoid people, places and situations that might be anxiety-provoking
- I have allowed my loved one to cancel plans that they feel triggered by
- I have helped my loved one avoid being on their own I have held myself back from saying or doing things that might have triggered my loved ones’ anxiety
- I have avoided tackling my loved ones’ anxiety and OCD patterns because it causes them too much distress
- I helped my loved one avoid unpleasant thoughts, emotions and memories that might trigger their OCD
- I have made excuses for my loved one so that they would not have to face difficult situations
Reassurance-seeking
- I repeatedly use logical arguments to persuade and convince my loved one that their fears are unfounded
- I have tried to help my loved one be 100% certain
- I get caught up in the details of what my loved one said about the problem
- I have repeatedly provided reassurance in response to my loved ones’ problem
- I have repeatedly gotten caught up in the same unhelpful discussions about my loved ones’ anxieties or intrusive thoughts
- I have tried to persuade my loved one that they are not in danger
- I have engaged in intellectual discussions to try and reduce their anxieties at the expense of helping my loved one work through their emotions about the situation
Changing behaviours
- I have altered my routines, such as chores, to accommodate my loved ones needs
- I have completed tasks for my loved one that they try to avoid
- I wash my hands or other items more frequently than necessary
- I have given in to requests or demands made by my loved one, which they wouldn’t normally make
- I have assisted my loved one with things they should be able to do themselves, for example dressing, eating or walking
- I have given my loved one things they wouldn’t need without their OCD, for example cleaning products
- I have waited for my loved one to carry out rituals related to their anxieties
- I have performed chores for my loved one that they should have done themselves
- I have changed my normal routines in response to my loved ones’ anxieties, for example not going to work or changing the family’s routines
What can I do to offer my loved one support and not reassurance?
Not engaging in reassurance-seeking behaviour that your loved one requests will feel like the exact opposite of what you want to do. However, research shows that individuals with OCD who receive reassurance from family, involve them in rituals, or engage them in avoidance behaviours often experience poorer treatment outcomes. On the contrary, resisting the urge to provide reassurance and instead supporting your loved one in disengaging from compulsions has been shown to improve outcomes for people with OCD.
So how can you do that?
- Understanding the difference between assurance and reassurance: Assurance is making sure of something, like if you turned the stove off, and is a natural reaction when there is doubt. Reassurance is making sure of something, again and again and again. This reassurance might become a compulsion for someone with OCD, requiring them to do certain mental or physical rituals in response to their doubt. Therefore, the thing to be aware of is the repetitiveness. You should focus on encouraging your loved one to not keep seeking reassurance about the same doubts.
- Acknowledge that OCD is experienced differently for those living with or without it: OCD is perceived differently based on whether it is first-hand lived experience or externally viewed by a loved one. It is important to understand that your loved ones’ OCD makes them believe their fears are true and that it is necessary to perform certain behaviours. While you might see these behaviours as unnecessary, irrational and unimportant, it is crucial to acknowledge that individuals with and without OCD have different experiences. This will help your loved one not feel misunderstood.
- Make your loved one aware of their safety behaviours: People with OCD may not always be aware of their safety behaviours, despite it likely being very obvious to you. You should ask your loved one questions about particular safety behaviours they are frequently performing and why they feel the need to perform these behaviours. These conversations should not be had when your loved one is in a highly anxious state and should instead take place with a gentle tone and calm environment.
- Provide emotional support when your loved one is in a very anxious state: Providing words of encouragement and recognising the difficulty that your loved one is going through especially in moments of high fear can be incredibly powerful. It might help to explain that if you accommodate their behaviour, it will only worsen their OCD. However, in saying this, sometimes when you’re caring for someone in a highly anxious state, you might need to go along with the reassurance-seeking and accommodations just to get through the day. If they’re in treatment, encourage your loved one to talk about the situation with their therapy team. And if they’re not in treatment, it might be time to have a conversation about professional support.
- Create a safe space for your loved one: Research suggests that individuals are more likely to work on challenging their intrusions and compulsions if they can voice them in an accepting environment, whereas they are more likely to engage in compulsions in triggering situations.
- Give positive feedback to your loved one after an exposure task: Exposure and response prevention (ERP) is the gold-standard treatment for people living with OCD. It involves purposefully exposing someone with OCD to people, places and situations that make them anxious with the aim of retraining their brain to no longer see the obsession as a threat. ERP should be done with careful planning and under the guidance of a therapist but providing positive and supportive feedback to your loved one when they complete an ERP task has been shown to reduce reassurance behaviours compared to those who provided neutral responses.
- Acknowledge all progress, even small progress: Similar to providing positive feedback to ERP tasks, fighting OCD is incredibly hard work for your loved one. It involved doing exactly the opposite of what helps them feel safe, good and reduce their anxiety. Acknowledging even the smallest of progress should be a cause for celebration.
What is your responsibility and what is your loved one’s responsibility?
With professional support, recovery from OCD is absolutely possible. But this is often a long and difficult road with you and your loved one having different responsibilities throughout the process. Below are some things to be aware of as you go through this this journey.
The responsibility of someone with OCD
- To get better and put in the hard work to make this possible
- To make changes to their behaviour
Your responsibility as a loved one
- Look after yourself
- Offer emotional support not reassurance
- It is not your responsibility to make your loved one feel better
- Maintain a relationship with your loved one outside of their condition
- Set healthy boundaries, especially when it comes to reassurance-seeking and accommodations
Not providing reassurance or engaging in accommodations for your loved one will feel like the exact opposite thing that you should be doing. However, this is the best thing for your loved one in the long-term. Remember, you are not alone and support is available.
Looking for support for OCD?
If you are looking for further support for a loved one, our team are here to discuss your options.
We have two specialist pathways for OCD treatment:
The first step is to have an assessment with a consultant psychiatrist. You can submit an enquiry form here and our team will be in touch with you to organise this appointment.
Related Conditions
Treatment approaches
Relevant specialists
-

Professor David Veale
Lead consultant for OCD and related disorders at Nightingale Hospital